Semaglutide, a GLP-1 receptor agonist, offers a convenient once-weekly injection for managing type 2 diabetes, effectively lowering HbA1c and reducing hypoglycemia risks. Regular follow-up appointments are crucial for optimizing its efficacy, monitoring side effects like gastrointestinal issues, and addressing patient non-adherence. Blood glucose level testing is essential for evaluating treatment outcomes. Effective patient education, including simplified explanations, support systems, and digital health technologies, enhances long-term adherence to semaglutide injectable form regimens. Future advancements aim to improve patient convenience with pre-filled syringes, autoinjectors, and remote monitoring apps.
Regular follow-ups are essential for optimizing the efficacy of semaglutide, a game-changing medication delivered via its injectable form. This comprehensive guide explores the critical role of scheduled check-ins in ensuring optimal treatment outcomes. From understanding semaglutide’s mechanism to monitoring patient compliance and managing side effects, each section delves into essential aspects of effective semaglutide injection management. By the end, readers will grasp the significance of regular follow-ups in maximizing the benefits of this innovative therapy.
Understanding Semaglutide and its Injectable Form
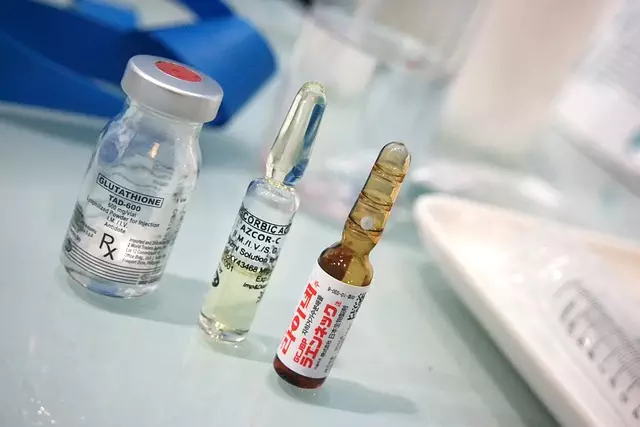
Semaglutide, a type of glucagon-like peptide-1 (GLP-1) receptor agonist, has gained significant attention in diabetes management due to its unique properties and benefits. Its injectable form offers a novel approach to regulating blood sugar levels compared to traditional insulin injections. This medication mimics the natural hormone GLP-1, which is produced by the gut in response to food intake, stimulating insulin secretion and suppressing glucagon release.
The semaglutide injectable form is administered once weekly, providing a convenient alternative to more frequent insulin dosing. It has shown remarkable efficacy in lowering HbA1c levels, improving glycemic control, and reducing the risk of hypoglycemia in individuals with type 2 diabetes. Additionally, its long-acting nature allows for sustained blood sugar regulation throughout the day, making it a promising treatment option for those seeking better diabetes management.
The Role of Regular Follow-ups in Injection Efficacy
Regular follow-up appointments play a pivotal role in optimizing the efficacy of injection therapies, especially with the rise of innovative forms like semaglutide, an injectable medication. These scheduled check-ins allow healthcare professionals to monitor patient responses, ensuring the treatment stays on track and addressing any potential issues promptly. By assessing the body’s reaction to injections, such as those containing semaglutide, medical experts can make informed adjustments to dosage or treatment frequency, maximizing benefits while minimizing risks.
Through these follow-ups, patients receive personalized guidance, and their concerns are addressed. It fosters a collaborative relationship between patients and caregivers, enhancing adherence to the prescribed injection regimen. This proactive approach not only improves clinical outcomes but also contributes to better patient satisfaction and long-term management of conditions treatable by semaglutide injectables.
Identifying Potential Side Effects and Adverse Reactions

Regular monitoring of injection efficacy is crucial, especially with the growing popularity of semaglutide in its injectable form. While generally well-tolerated, this medication can cause potential side effects and adverse reactions that should not be overlooked. Common issues include gastrointestinal problems like nausea, vomiting, or diarrhea, which may impact a patient’s quality of life.
Healthcare providers must encourage patients to report any unusual symptoms promptly. Serious reactions, although rare, can occur, such as pancreatitis or kidney issues. Staying vigilant and conducting thorough follow-ups allows for early detection and management of these reactions, ensuring the best possible outcomes for individuals receiving semaglutide injections.
Monitoring Patient Compliance and Adherence to Treatment

Regular follow-ups are essential for monitoring patient compliance and adherence to treatment, especially with semaglutide, a popular injectable form of medication. Healthcare providers play a crucial role in ensuring patients understand the importance of consistent dosing and timely injections. During these check-ins, professionals can assess if individuals are adhering to their prescribed regimens, offer guidance on any challenges they might face, and address concerns or misconceptions about semaglutide therapy.
Through these interactions, healthcare teams can identify potential issues that may hinder treatment success, such as missed doses or difficulties in administering injections. They can then provide tailored solutions, educational resources, or support to enhance patient adherence. Regular monitoring facilitates timely interventions, ultimately improving injection efficacy and patient outcomes associated with semaglutide use.
Evaluating Blood Glucose Levels and Glycemic Control

Regular monitoring of blood glucose levels is an integral part of managing diabetes and assessing the efficacy of injection treatments, including semaglutide in its injectable form. This process allows healthcare professionals to gain valuable insights into how well the body is regulating blood sugar levels. By evaluating glycemic control, they can make informed decisions about adjusting medication dosages or treatment plans.
For patients receiving semaglutide injections, regular testing enables them to track improvements or changes in their metabolic health. It helps identify if the injectable form of semaglutide is effectively lowering blood glucose levels and maintaining a stable glycemic range. This continuous assessment is crucial for preventing hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar), both of which can have severe consequences on overall health and daily well-being.
Adjusting Dose and Addressing Treatment Challenges

Regular follow-ups are essential for optimizing the efficacy of injection treatments, especially with semaglutide in its injectable form. During these visits, healthcare providers can closely monitor patients’ responses and adjust doses as needed. This tailored approach is crucial when managing conditions like type 2 diabetes or obesity, where semaglutide’s long-term effects vary between individuals. By regularly assessing treatment outcomes, providers can ensure optimal drug concentrations, minimizing the risk of adverse reactions while maximizing therapeutic benefits.
Treatment challenges often arise due to patient non-adherence or unique metabolic profiles. For instance, some patients may struggle with consistent injection schedules or experience side effects that impact their quality of life. In such cases, healthcare professionals should explore alternative delivery methods, discuss patient concerns, and consider personalized treatment plans. Regular follow-ups empower providers to navigate these challenges, ensuring patients receive the most effective and suitable semaglutide therapy.
Enhancing Patient Education and Support Systems

Effective patient education is a cornerstone in ensuring long-term adherence to injection regimens, particularly for complex medications like semaglutide, an injectable form used in diabetes management. Healthcare providers should take the time to educate patients about their condition and the treatment, including the benefits and potential side effects. Simple, clear explanations can help patients feel more comfortable with self-injecting and reduce barriers to adherence. Providing written resources, demonstrative training, and ongoing support can significantly enhance patient understanding and confidence in managing their diabetes.
Furthermore, building a robust support system around the patient can greatly contribute to treatment success. This includes encouraging family involvement, connecting patients to support groups or online communities, and ensuring access to reliable healthcare services. Regular follow-up appointments allow healthcare providers to monitor progress, address concerns, and offer tailored advice, fostering a collaborative environment that prioritizes patient well-being and adherence to injection protocols for medications like semaglutide.
Future Trends in Semaglutide Injection Management

The future of Semaglutide injection management looks promising, with innovations aimed at enhancing both patient convenience and treatment adherence. One notable trend is the development of improved semaglutide injectable forms, such as pre-filled syringes and autoinjectors, which can simplify the administration process and reduce errors. These devices offer precise dosing, easy handling, and some even come with built-in safety features to prevent accidental injections.
Additionally, digital health technologies are poised to play a significant role in semaglutide therapy. Mobile applications and wearable sensors can facilitate remote monitoring of patient outcomes, providing healthcare providers with real-time data on medication adherence and glucose control. This enables timely interventions and adjustments to treatment plans, ultimately improving long-term patient outcomes.