Semaglutide, a once-weekly injectable therapy for type 2 diabetes, effectively regulates blood sugar and aids weight management. Regular monitoring of blood glucose levels post-injection is crucial for optimal diabetes control, preventing complications, and optimizing insulin sensitivity. Home setup with reliable equipment ensures accurate readings, empowering patients to make informed decisions regarding diet, exercise, and medication adjustments. Understanding blood sugar metrics and seeking medical advice for persistent issues are key to successful management using semaglutide injectable form therapy.
Monitoring blood sugar levels after a Semaglutide injectable form is crucial for managing diabetes effectively. This article guides you through understanding Semaglutide, its benefits, and how to set up accurate home monitoring. We explore key benefits of regular tracking, offer tips for consistent measurement, and explain common challenges. Learn when to seek medical advice post-injection to ensure optimal health outcomes.
Understanding Semaglutide and Its Injectable Form
Semaglutide is a medication primarily known for its role in managing type 2 diabetes. It mimics a natural hormone, GLP-1, which helps regulate blood sugar levels by stimulating insulin release and suppressing glucagon production. The injectable form of semaglutide offers a convenient and effective way to control diabetes. This formulation is designed to be administered once weekly, providing long-lasting effects and reducing the need for frequent injections.
The semaglutide injectable form is often prescribed as a treatment option due to its ability to significantly lower blood sugar levels and improve overall glycemic control. Its unique mechanism of action not only aids in weight management but also reduces the risk of various diabetes-related complications. This medication has gained recognition for its potential to enhance quality of life for individuals living with type 2 diabetes.
The Importance of Post-Injection Blood Sugar Monitoring

Monitoring blood sugar levels after receiving a semaglutide injectable form is an indispensable practice for several reasons. This process plays a pivotal role in managing diabetes, ensuring patients maintain stable glucose levels and preventing potential complications associated with inconsistent or elevated blood sugar. By frequently checking post-injection readings, individuals can make informed adjustments to their diet, medication, or physical activity routines to optimize insulin sensitivity and overall metabolic control.
Such monitoring is particularly crucial for those using semaglutide, known for its prolonged effects on reducing blood sugar. Understanding how the body responds to this injectable form helps patients and healthcare providers identify any trends or anomalies in glucose levels. This proactive approach allows for timely interventions, facilitating effective diabetes management and improving overall quality of life for individuals living with this chronic condition.
Key Benefits of Regular Monitoring

Regular monitoring of blood sugar levels, especially after receiving a semaglutide injectable form, offers numerous advantages for individuals managing diabetes. This practice empowers patients to gain profound insights into their bodily responses, enabling them to make informed decisions about their diet, physical activity, and medication dosing. By keeping close tabs on glucose levels, individuals can prevent severe peaks or drops, both of which pose health risks.
Moreover, consistent monitoring facilitates timely interventions, allowing for quick adjustments to treatment plans. This proactive approach can lead to improved glycemic control over time, reducing the likelihood of developing long-term complications associated with diabetes. Regular checks also provide valuable data for healthcare professionals, enabling them to tailor recommendations and optimize patient care.
Setting Up for Accurate Monitoring at Home

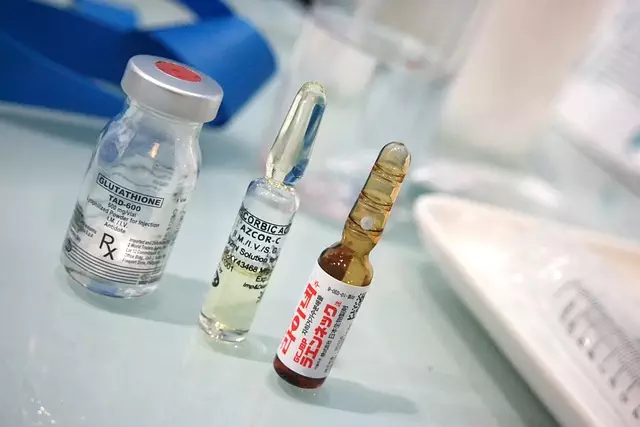
To ensure accurate monitoring of blood sugar levels post-injection with semaglutide, the home setup plays a crucial role. The first step is to obtain reliable blood glucose meters designed for at-home use. These devices should offer precise readings and be easy to operate, as consistency in testing procedures is essential. Calibrating the meter with regular control solutions provided by your healthcare provider ensures accurate results. Additionally, investing in lancing devices and test strips compatible with your chosen meter guarantees a seamless experience.
Next, create a designated area for monitoring at home. This space should be quiet, well-lit, and free from distractions to enable focused attention during tests. Ensure easy access to your injection site for quick blood samples. Regularly clean and sterilize your testing materials, especially lancets, to maintain hygiene and prevent contamination. By setting up an organized and clean environment, you can ensure that each monitoring session is efficient and yields accurate data, facilitating better management of your semaglutide injectable form therapy.
How to Perform Blood Sugar Tests After Semaglutide Injection

After receiving a semaglutide injection, it’s crucial to monitor your blood sugar levels regularly to ensure safe and effective diabetes management. The semaglutide injectable form is designed to mimic natural hormones, helping regulate glucose levels. To perform blood sugar tests accurately, start by checking your blood sugar level before the injection as a baseline. This can be done using a glucometer, which requires a small drop of blood from a finger prick.
Next, follow up with tests at specific intervals after the injection, typically at 2 hours, 4 hours, and 8 hours post-dose. These time points are critical as semaglutide’s effects can vary based on when it’s administered. Ensure you use a consistent testing method throughout to ensure accurate readings. Always consult your healthcare provider for personalized recommendations and guidance on adjusting insulin doses or treatment plans based on your blood sugar test results from the semaglutide injection.
Interpreting Results: What Numbers Indicate?

When monitoring blood sugar levels after a semaglutide injectable form, understanding the results is key to managing diabetes effectively. The primary focus is on glucose readings, typically measured using a blood glucometer. Ideal numbers vary based on individual health status and medical advice but generally, fasting blood sugar levels should be below 100 mg/dL (5.6 mmol/L), while post-meal readings should peak around 140 mg/dL (7.8 mmol/L) or less after two hours.
Interpretation involves comparing current results with historical data and personal targets. Consistently elevated levels above the target range may indicate a need for adjustment in medication dosage, meal planning, or physical activity. Conversely, low blood sugar (hypoglycemia), often below 70 mg/dL (3.9 mmol/L), requires immediate action to restore balance. Keeping track of these numbers helps healthcare providers and individuals make informed decisions about diabetes management.
Common Challenges and Tips for Consistent Monitoring

Monitoring blood sugar levels after receiving a semaglutide injectable form can be challenging, but consistent tracking is crucial for managing diabetes effectively. One common obstacle is maintaining adherence to regular testing routines. Many individuals struggle with the daily commitment required to monitor levels at various times, especially when adjusting to new treatment plans. However, establishing a structured schedule and setting reminders can help overcome this challenge. Using apps or devices designed for glucose monitoring can also make the process more manageable and user-friendly.
Additionally, maintaining consistent pre-injection routines is essential. This includes preparing supplies in advance, ensuring easy access to test strips and lancets, and familiarizing oneself with proper injection techniques. Accurate readings depend on clean and correct needle insertion, so practicing good hygiene and following healthcare provider instructions for storage and usage is vital. Addressing these common challenges can empower individuals to consistently monitor their blood sugar levels, leading to better diabetes management and improved overall health outcomes.
When to Seek Medical Advice Post-Injection

After receiving a semaglutide injectable form, it’s crucial to be vigilant about your blood sugar levels. If you experience persistent high blood sugar (hyperglycemia) or low blood sugar (hypoglycemia), it’s important to seek medical advice promptly. Hyperglycemia is particularly concerning as it could indicate an adverse reaction to the medication or underlying diabetes management issues. Symptoms of hyperglycemia include increased thirst, frequent urination, and fatigue.
On the other hand, hypoglycemia can be equally distressing and requires immediate attention. Signs may include dizziness, sweating, rapid heartbeat, and confusion. If you notice any of these symptoms, especially within a few hours after injection, contact your healthcare provider right away. They can guide you on the next steps, which may involve adjusting your medication dose or providing additional treatment to bring your blood sugar levels back to a safe range.



